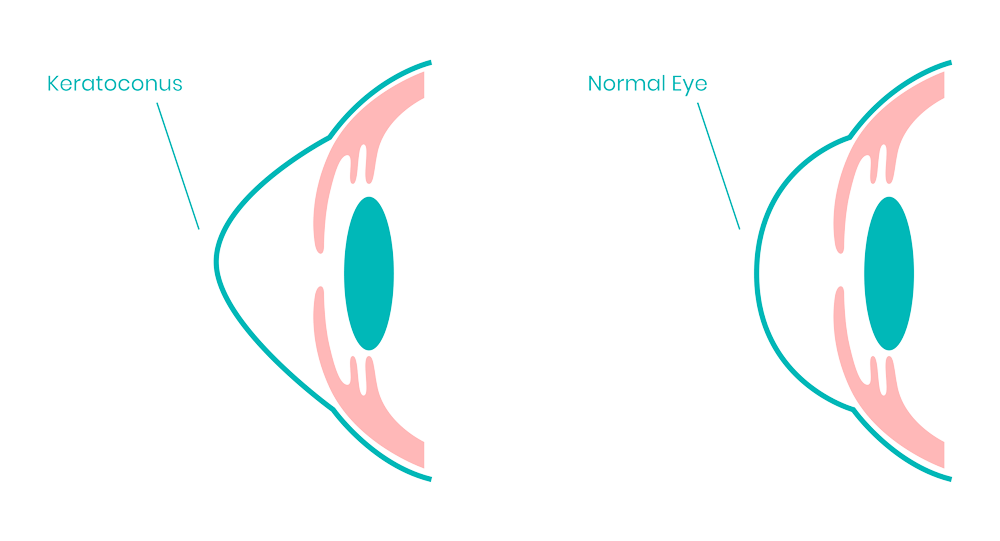
Cornea is the outer covering of the eyeball. Protecting structures within the eye is the primary purpose of this coat. In addition to acting as a structural barrier, the cornea also protects the eye from infection. Combined with the tear film, it provides a proper anterior refractive surface for the eye. The cornea contributes two-thirds of the eye's refractive power.