
Get expert cornea care and advanced keratoplasty treatment in Ahmedabad
Book an Appointment
A corneal ulcer is an inflammation of the cornea that can cause eye pain, redness, excessive tearing, blurred vision, and sensitivity to light. The most common corneal ulcer causes include eye injuries, dirty contact lenses, viral infections, and exposure to contaminated water. While infections are the leading cause, trauma to the eye can also result in an eye ulcer. If you experience corneal ulcer symptoms, such as a white spot on the cornea, swelling, or discomfort, seek immediate medical attention to prevent vision loss.

Common symptoms of corneal ulcer are:
A corneal ulcer is an open wound on the cornea, often caused by bacterial, viral, or fungal infections. Other corneal ulcer causes include dry eyes, eye injuries, or improper contact lens use. Among the types of corneal ulcers, bacterial corneal ulcers are common in contact lens users, while viral keratitis, caused by the herpes simplex virus, can lead to recurring ulcers. Common corneal ulcer symptoms include eye pain, redness, blurred vision, excessive tearing, and light sensitivity. If untreated, an eye ulcer can lead to corneal scarring and vision loss. Corneal ulcer treatment depends on the cause—antibacterial, antifungal, or antiviral eye drops. Viral ulcers may recur despite treatment. In severe cases, Cornea & Keratoplasty Treatments (corneal transplant) may be needed. Early diagnosis and treatment are essential to prevent vision loss. Proper eye care and timely medical attention help avoid complications.
The picture shows a corneal ulcer with a positive fluorescein stain, which is commonly used to confirm the diagnosis of a corneal ulcer. The greenish-yellow stained area indicates the loss of the outermost corneal layer in that region.
With immediate treatment, most corneal ulcers can heal without vision loss. However, if the infection is left untreated or becomes too severe, it can cause permanent damage to the eye.

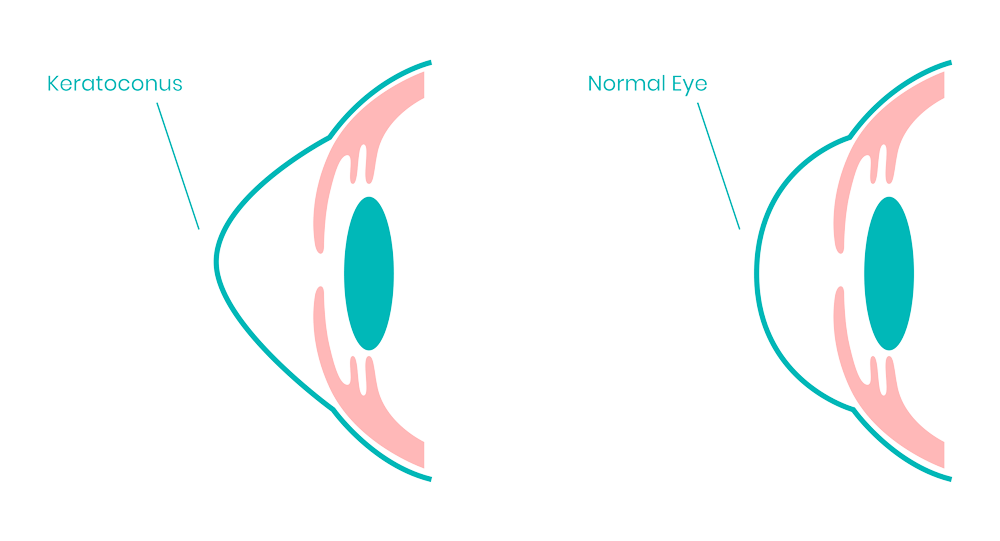
Keratoconus is a condition where the front part of the eye, called the cornea, becomes thin and starts to bulge outward in a cone shape. This can make vision blurry or distorted. At first, the bulge may be small, but it can get worse over time. In most cases, both eyes are affected, leading to increasing vision problems. In India, about one in every 2,000 people has keratoconus. It usually starts in teenagers or young adults, often in their mid-teens or early twenties. Frequent eye rubbing is a common cause that can make the condition worse. Early detection is important for managing keratoconus. Treatment options include special contact lenses, a procedure called corneal cross-linking to strengthen the cornea, and in severe cases, a corneal transplant. Regular eye check-ups can help detect keratoconus early and prevent further vision loss.
Many keratoconus patients are unaware of their condition, as the earliest symptom is mild blurry vision or progressively worsening eyesight that is not easily corrected. Due to a lack of awareness, many cases remain undiagnosed. If a person experiences frequent changes in spectacle power along with reduced corneal thickness, a corneal topography test is recommended to rule out keratoconus. In the early stages, there may be no noticeable symptoms apart from a gradual decline in vision. However, in later stages, additional symptoms may develop, such as increased light sensitivity, glare, and distorted vision. Whereas, in late stages following symptoms can be noted:
Glare and halos around lights
Difficulty seeing at night
Eye irritation or headaches associated with eye pain
Increased sensitivity to bright light
Sudden worsening or clouding of vision
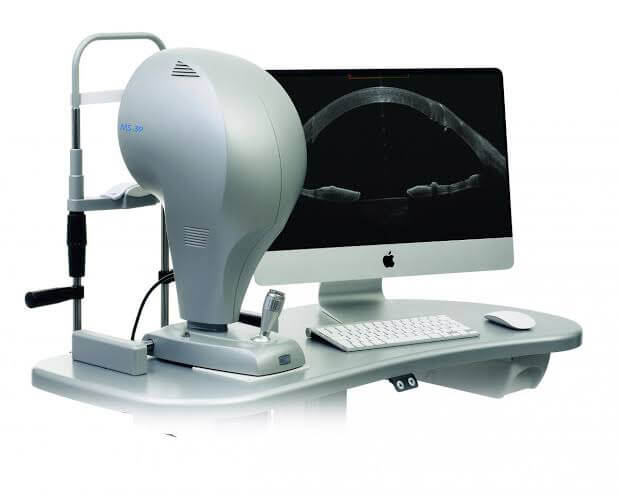

MS-39 is the most advanced device for analyzing the anterior segment of the eye. It combines Placido disk corneal topography with high-resolution OCT-based anterior segment tomography for precise diagnostics.
In the early stages of keratoconus, spectacles can help correct vision. As the condition progresses, individually fitted ROSE K contact lenses are needed, as they provide better vision. However, some patients may experience increased sensitivity to glare and light. Finding well-fitting lenses can be challenging, but they must be comfortable to wear. Poorly fitting lenses can cause discomfort and may further damage the cornea.
Cross-linking the cornea (C3-R) is another treatment option that does not require invasive surgery. This procedure strengthens the cornea, preventing the bulge from worsening, though it does not reverse the existing shape.
A more advanced treatment for keratoconus is topo-guided C3R. In this procedure, an excimer laser is used to smooth the cone-shaped cornea before performing collagen cross-linking (C3R) to enhance corneal strength. This technique not only stops the progression of the bulge but also improves functional vision.

A pterygium is a growth of the conjunctiva or mucous membrane that extends from the white part of the eye onto the cornea, the clear front covering of the eye. This benign (noncancerous) growth is often wedge-shaped and usually does not cause significant problems. However, if it grows large enough to interfere with vision or cause discomfort, it may require treatment or surgical removal.
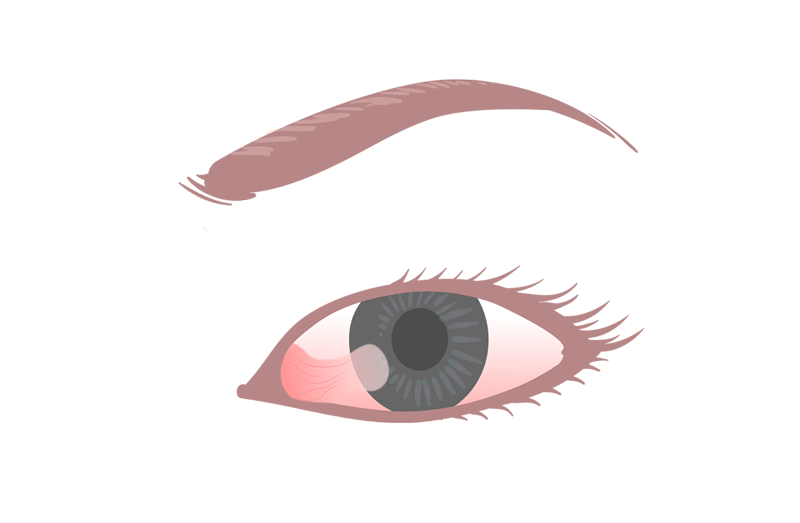
A pterygium does not always cause symptoms, but when it does, they are usually mild. Common symptoms include redness, blurred vision, and eye irritation, along with a burning sensation or itchiness. If the growth becomes large enough to extend over the cornea, it can interfere with vision. A thick or enlarged pterygium may also create a sensation of having a foreign object in the eye. Additionally, wearing contact lenses may become uncomfortable or even impossible due to irritation and discomfort.
Cornea transplantation is a surgery used to replace a damaged cornea with a healthy, donated one. Some surgeries remove the entire cornea, while others only remove a few parts. The surgery is used to treat a few different corneal diseases. It is often the best way to treat infection and save sight.

The outcome of corneal transplantation depends on the underlying cause of corneal damage. Most patients experience at least some vision improvement, and in many cases, the surgery is highly successful. Regular follow-up visits are essential to ensure proper healing and prevent complications. A corneal transplant is recommended if the cornea is severely damaged due to: